Goa is abuzz with excitement as vintage bike and car owners, users, collectors and fans are decking […]

TEST. TREAT. TRIUMPH – THE THALASSEMIA TALK
May 10- May 16, 2025, MIND & BODY, HEART & SOUL May 9, 2025Q&A interview with Dr Amit Dias on World Thalassemia Day
On World Thalassemia Day observed on May 8, as the world stands in solidarity with those affected by this inherited blood disorder. Public health researcher Dr Amit Dias has worked on the quality of life of children with thalassemia in Goa and in this tell-all chat, he uncovers what thallasemia is, why it matters, how it’s treated, and — most importantly — how it can be prevented. He says, “ We need to test, treat and triumph” in this informative interview. We learn how to untangle the genes, unpack the facts, and understand why a little awareness can save a lot of pain…
Goan Observer: Let’s start with the basics — what exactly is thalassemia?
Dr Amit Dias: Thalassemia is a genetic blood disorder that affects the body’s ability to produce hemoglobin, the protein in red blood cells that carries oxygen. In thalassemia, the red cells are either defective or produced in lower numbers, leading to anemia. There are two main types based on the affected globin chain:
Alpha Thalassemia: Caused by mutations in the genes that produce alpha globin chains.
Beta Thalassemia: Caused by mutations in the genes that produce beta globin chains. This is more common in India and includes:
Thalassemia Major: The most severe form, where both beta globin genes are defective, leading to severe anemia from early childhood. These patients require lifelong regular blood transfusions and iron chelation therapy.
Thalassemia Intermedia: A moderate form with less severe anemia; transfusions may be needed occasionally.
Thalassemia Minor (Trait): A mild, carrier state. Individuals may have mild anemia but generally lead normal lives and may be unaware they are carriers.
Thalassemia is particularly common in regions where malaria was or is prevalent, including parts of India, the Mediterranean, the Middle East and Southeast Asia.
Q: What do we need to do about it?
A: We all need to be aware about it. We need to test, treat and triumph.
Test – Promote early screening and carrier detection
Treat – Ensure access to quality care for those affected
Triumph – Work together toward prevention and cure
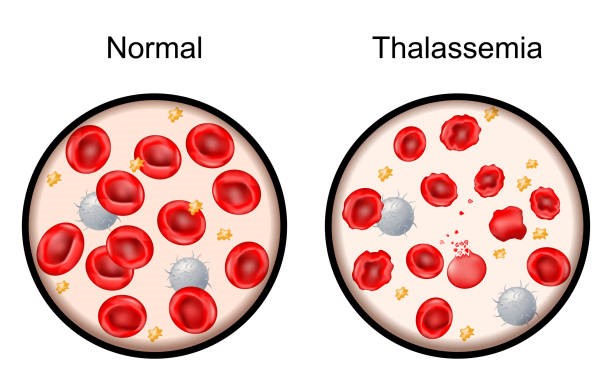
Q: What is the blood look like in a person with thalassemia?
A: The peripheral blood smear depends on the type of disorder, the cells and test results — especially in thalassemia major — are distinct and are helpful in the diagnosis. The peripheral smear will show the following.
Microcytic hypochromic red cells: RBCs are small (low MCV) and pale due to low hemoglobin content.
Target cells: Red cells with a bull’s-eye appearance, due to excess membrane relative to cell volume.
Anisopoikilocytosis: Variation in size (anisocytosis) and shape (poikilocytosis) of red cells.
Nucleated red blood cells (normoblasts): Seen in severe cases due to increased erythropoietic activity in the bone marrow and extramedullary sites.
Basophilic stippling: Indicates abnormal RNA aggregation in red cells.
Tear drop cells and fragmented cells may also be present.
Q: How is this trail passed on genetically?
A: This could a bit complicated, but let me simplify it. Thalassemia follows an autosomal recessive pattern, meaning a child needs to inherit the defective gene from both parents to develop thalassemia major. If only one gene is inherited, the person becomes a carrier or has thalassemia minor — usually with no symptoms but capable of passing the gene to offspring.
This is why carrier screening and genetic counseling are vital, especially before marriage or planning children.
Q: How big a problem is thalassemia in India — and is it a concern in Goa? Tell us about your research.
A: India has over 100,000 people living with thalassemia major, and about 10,000–15,000 babies are born each year with the condition. Around 3 to 4% of the Indian population are carriers. That’s over 40 million people!
Yes, it’s very much a concern in Goa. In fact, our study — GOTQol (Goa Thalassemia Quality of Life Study)—highlighted the quality of life and the physical, emotional, social and financial impact of thalassemia on children and their families right here in the state.
Q: What did your study on thalassemia reveal about the quality of life of children with the condition in Goa?
A: The GOTQoL study, or the Goa Thalassemia Quality of Life study, published in the International Journal of Contemporary Pediatrics, meticulously evaluated the quality of life in children afflicted with thalassemia major attending a tertiary care center in Goa.
The research was conducted by Dr Ankusk, Dr Mimi Silveira and myself (Dr Amit Dias), in collaboration with my students Joachim and Yash. The findings revealed that these children experienced a significantly diminished quality of life compared to their healthy counterparts, particularly in the domains of physical, social, and academic functioning.
Additionally, they exhibited lower psychosocial and overall health summary scores. Notably, children undergoing chelation therapy and those with well-informed parents demonstrated enhanced physical functioning. The study underscores the imperative for accessible chelation therapy, parental counseling, and collaborative support from healthcare providers, educational institutions, and policymakers to bolster the well-being of children with thalassemia. They received care from the department of pediatrics, which had devised innovative approaches and established protocols to prioritize the patients.
Q: How are those affected by Thalassemia treated?
A: The mainstay is regular blood transfusions, often every 2–4 weeks. These help maintain adequate hemoglobin levels. But there’s a catch — iron overload.
Hence, patients also need iron chelation therapy to remove excess iron that accumulates in organs due to repeated transfusions. In some cases, bone marrow or stem cell transplantation is a curative option, though costly and limited by donor availability.
Q: What are the complications of repeated blood transfusions in thalassemia?
A: Repeated transfusions lead to iron overload, damaging organs like the heart, liver, and endocrine glands, leading to diabetes, cardiac issues, and growth problems. One needs to carefully monitor them and ensure that this is treated. There’s also the risk of infections like hepatitis B and C, though screening has improved.
Q: Is thalassemia considered a disability in India?
A: Yes. Under the Rights of Persons with Disabilities (RPwD) Act, 2016, thalassemia is recognized as a benchmark disability. This ensures access to reservations, free treatment, and support for education and employment. It’s a crucial step in mainstreaming patients and improving quality of life.
Q: Why is World Thalassemia Day observed on May 8?
A: It’s observed in memory of George Englezos, the son of Thalassemia International Federation founder Panos Englezos, who passed away due to the condition. It’s a day to honor patients, parents, and advocates and to remind us of the importance of awareness, prevention, and care. The theme this year is “Uniting Communities & Prioritising Patients.”
Q: What happens if thalassemia is left untreated?
A: If untreated, children with A: thalassemia major may develop severe anemia, organ failure, growth retardation, and early death, often before adolescence. Early diagnosis and lifelong treatment are essential for survival and health.
Q: Can thalassemia be prevented?
A: Absolutely. The most powerful tool is prevention. This includes:
Carrier screening, especially before marriage.
Pre-natal diagnosis in at-risk couples.
Public awareness programs.
Countries like Cyprus and Iran have successfully brought down thalassemia births to near zero using nationwide screening. India can do it too.
Q: Are there newer therapies for thalassemia patients?
A: Yes, there’s exciting progress. Gene therapy, where the faulty gene is corrected or replaced, is emerging as a potential cure. Also, gene editing (CRISPR) is being explored. While costly now, these therapies offer hope for a transfusion-free life in the future.
Q: Your message for World Thalassemia Day?
A: Let’s unite as a community, prioritize the patients, and prevent future suffering. A simple blood test before marriage can save a lifetime of pain. To every patient and caregiver out there — you are not alone, and together, we can break the chain.
Let’s make Thalassemia Day not just a reminder — but a revolution.