An interview with Dr Amit Dias
ON World Parkinson’s Day we spoke to DR AMIT DIAS to get a better understanding of Parkinson’s disease. “There is much more than what we see,” he explains, as he reveals the iceberg phenomenon in Parkinson’s disease. “We need to break all barriers and provide comprehensive care to patients of Parkinson’s disese.” Read this informative interview and spread awareness.
Goan Observer: Why is April 11 observed as World Parkinson’s Day?
Dr Amit Dias: April 11 is the birthday of Dr James Parkinson, who first described the disease in 1817. It’s observed globally to raise awareness about Parkinson’s and honor Dr Parkinson’s contribution to understanding this condition. He published his findings in an article titled “An Essay on the Shaking Palsy.”
Q: What exactly is Parkinson’s disease?
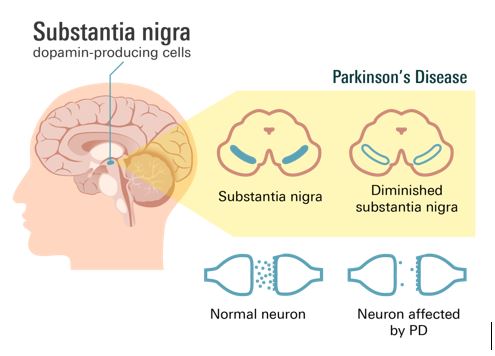
A: Parkinson’s disease is a progressive nervous system disorder that affects movement. In this condition, there is a gradual loss of dopamine-producing cells in a region of the brain called the substantia nigra. This loss leads to abnormal brain activity, causing the characteristic symptoms of Parkinson’s.
It develops gradually, often starting with a barely noticeable tremor in one hand. Over time, it can cause stiffness or slowing of movement.
Q: What is the burden of Parkinson’s disease in the world and India?
A: Parkinson’s affects approximately 6.3 million people worldwide and its prevalence is increasing due to aging populations. In India, the numbers could be above 10 lakh. However, we need to accept that the actual number could be higher due to under reporting and lack of awareness.
Q: What are the signs and symptoms of Parkinson’s disease?
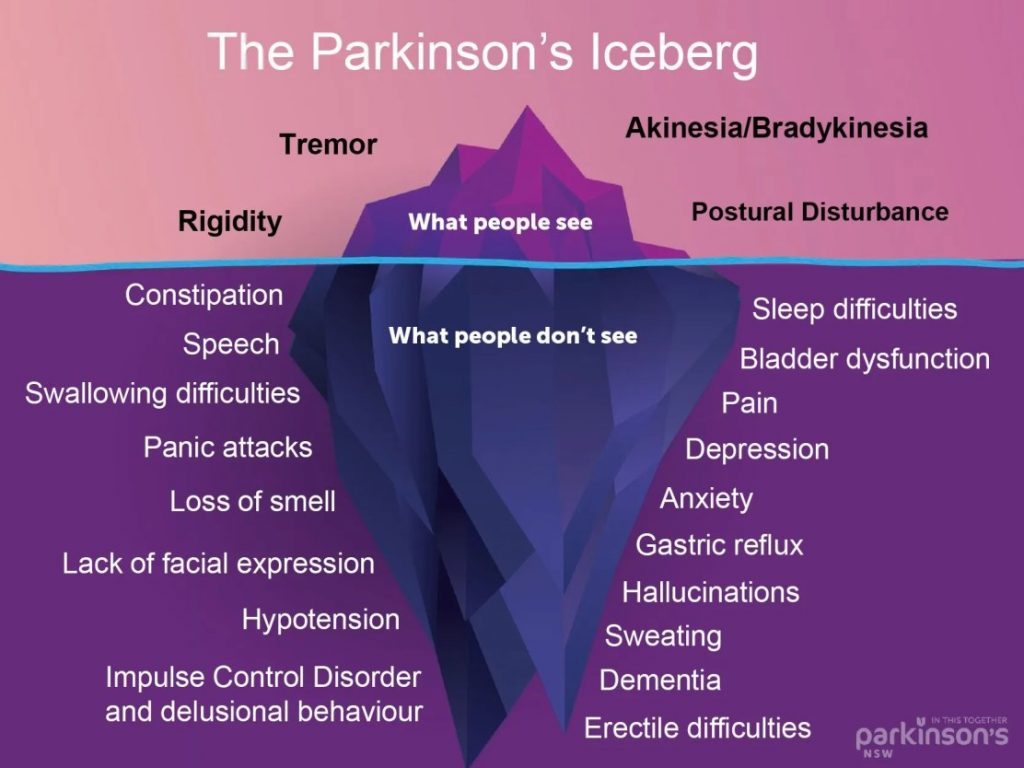
A: With close to 50 symptoms, the complexity of Parkinson’s is severely underestimated. The recognizable symptoms of Parkinson’s are just the tip of the iceberg. Beneath the surface, there are more than 20 non-motor symptoms ranging from being irritating and disturbing to life-threatening.
Tremors: Typically starting in one hand, tremors are one of the most recognizable symptoms of Parkinson’s. They often occur at rest and may decrease with intentional movement.
Bradykinesia: Slowness of movement is another hallmark symptom. Patients may have difficulty initiating movement, and their movements may become smaller and slower over time.
Muscle Stiffness: Rigidity or stiffness in the muscles can occur, making movement and tasks such as getting out of a chair or turning in bed more challenging.
Postural Instability: Parkinson’s patients may experience difficulty with balance and coordination, leading to a stooped posture and an increased risk of falls.
Freezing of Gait: Some individuals with Parkinson’s disease may experience sudden, temporary inability to move their feet forward while walking, feeling as though their feet are glued to the ground.
Speech Changes: Speech may become softer, slower, or more monotone, and patients may have difficulty with articulation or finding the right words.
Loss of Automatic Movements: Patients may experience a reduction or loss of automatic movements such as blinking, swinging arms while walking, or smiling.
Micrographia: Handwriting may become smaller and more cramped, a symptom known as micrographia.
Masked Face: Reduced facial expressions or a “mask-like” appearance of the face is common in Parkinson’s disease.
Q: You mentioned the “risk of falls” in people with Parkinson’s disease due to instability. Is there a way one can prevent it?
A: Yes, it’s vital to be aware of the risk of falls and take measures to prevent them.
Here are some general guidelines.
Preventing falls in Parkinson’s disease patients requires a multifaceted approach that addresses various factors contributing to the risk of falls. Here are some detailed tips:
Medication Management: Ensure that the patient takes their Parkinson’s medications as prescribed. Fluctuations in medication levels can affect balance and mobility.
Physiotherapy: Regular physiotherapy sessions can improve balance, strength, flexibility, and gait in Parkinson’s patients.
Home Safety Modifications: Remove tripping hazards such as loose rugs, clutter, electrical cords, and low-lying furniture from the home environment. Install grab bars in the bathroom and near the toilet and shower to assist with stability and prevent falls. Ensure good lighting.
Assistive Devices: Encourage the use of assistive devices such as canes, walkers, or mobility scooters to provide stability and support during walking. People sometimes refuse to use them and prefer to show that they can move without support. However, they need to be made aware that assistive devices are meant for their safety and should be used.
Footwear: This should not be ignored. Advise the patient to wear supportive, low-heeled shoes with non-slip soles to improve traction and stability.
Environmental Modifications: Arrange furniture to create clear pathways for walking and ensure that there’s adequate space for movement around the house. Install nonslip mats or adhesive strips in the bathtub or shower to reduce the risk of slipping. Consider using raised toilet seats or shower chairs to facilitate safe and comfortable personal care activities.
Fall Detection and Alarm Systems: If available, install fall detection or alarm systems that can alert caregivers or emergency services in case of a fall. Wearable devices equipped with fall detection technology can provide an added layer of safety and peace of mind.
Regular Assessment and Monitoring: Monitor the patient’s condition regularly and assess for any changes in balance, gait, or mobility. Be aware of postural hypotension (sudden drops in blood pressure upon standing), which can increase the risk of falls, and consult with the healthcare provider if such symptoms occur. It can be due to the medications.
Education and Support: Educate both the patient and their caregivers about the risk factors for falls and strategies to prevent them.
Q: Is it a fatal disease?
A: Parkinson’s itself is not considered fatal, but complications arising from the disease, such as pneumonia or falls, can be life-threatening, especially in advanced stages. One should ensure proper treatment and comprehensive care.
Q: Can it be treated and cured? What are the treatment options?
A: While Parkinson’s has no cure, there are several treatment options available to manage symptoms. These include medications to increase dopamine levels such as L Dopa and carbidopa, deep brain stimulation surgery, and therapies such as physiotherapy and occupational therapy.
Q: Where can people with Parkinson’s disease get help?
A: It starts with getting a diagnosis. Visit your nearest health center or health and wellness center and consult them if you notice any of the signs mentioned above. Remember that all tremors are not Parkinson’s disease. If they suspect Parkinson’s disease, get a confirmed diagnosis from a physician or neurologist. The Neurology department at GMC runs an OPD on Tuesdays and Thursdays. There are NGOs such as the Parkinson’s Society of Goa that can provide support in the state. There are several reliable resources available on the internet. Parkinson’s Europe, World Parkinson’s Program, etc.
Q: What is the theme for World Parkinson’s Day 2024?
A: The theme for World Parkinson’s Day 2024 is “Breaking Barriers: Together We Can.” It emphasizes the importance of collaboration among patients, caregivers, healthcare professionals, and researchers to overcome the challenges posed by Parkinson’s disease.